I can stare in the mirror and recite, “Every day, in every way, I’m getting better and better,” and I will still experience my life as awful unless I also have opportunities to succeed or I live in a community where, by comparison, I am no worse off than others. Wellbeing is a social phenomenon (Ungar, 2014).
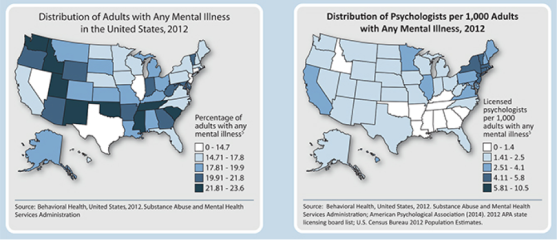
It is no secret that poverty and unemployment are highly correlated; however, it is somewhat less widely known that these factors mediate, and are influenced by, mental health. Recent research suggests that socio-economic hardship precedes inferior mental health (Heflin & Iceland, 2009). Commonly, mental health is associated with emotions and feelings including stress, depression and loneliness. On the other hand, mental illness is reserved by many for diseases and disorders such as schizophrenia, bipolar disorder, posttraumatic stress disorder, etc. The reality is that many diagnosable mental disorders are based on criteria regarding the factors considered by many to be a part of everyday life (i.e. stress, anxiety, alcohol, drug and even tobacco use). The Mayo Clinic estimates that one in five adults experience mental illness in a given year (2015). Furthermore, Kessler states that forty-six percent of Americans experience at least one mental disorder in their lifetime (as cited in Anakwenze & Zuberi, 2013, p.147). In either course, the mental state of an individual, and societies at large, have vast socioeconomic implications. Scholarly contributions from the United Kingdom suggest that the lowest wage-earners are twice more likely to experience mental health issues than average wage-earners and are more likely to experience unemployment (Kronenberg, Jacobs & Zucchelli, 2015). In 1997, William Julius Wilson found a relationship between poverty and mental health, of which, he concluded that unstable work and low income decrease self-efficacy (as cited in Anakwenze & Zuberi, 2013, p. 148). However, despite a rather lengthy history of research concerning the topic (which continues to be empirically vetted), there has yet to emerge a viable socio-economic prescription for mental illness. This review of literature focuses on determining the key socioeconomic factors associated with mental illness, and adds clarity to the relationship between poverty, unemployment and mental health.
Finding a place in society
As a part of the Fair Labor Standards Act in the U.S., the Wage and Hour Division of the Department of Labor [DOL] authorizes employers to pay subminimum wages to individuals who possess disabilities that effect job performance (2008). Mental illness is included among the list of impairments which qualify for a subminimum wage (DOL, 2008). Regardless of the intent, these standards imply a degradation of value to those with mental illness. The chasm between economical and humanistic thinking is evidenced by such government actions. That is, economically, individuals lose their name and their very identity (i.e. self-efficacy) and are considered in conventional terms, “factors of production”, “government expenses”, “buyers and sellers”, to name a few. Government intervention that provides a means for employers to pay individuals with mental illness less for jobs which they are less than qualified, does little to fix any economic or mental health dilemma. Efforts may better be served by providing resources, such as research endeavors purposed with determining suitable employment options for those with specific mental illness. Employing individuals in positions where their efforts and productivity are economically valuable to employers decreases the need for subminimum wage authorizations, and has potential to improve workers’ mental health and the business’ output. One challenge to this effort may be that individuals with serious psychological distress are more likely to have less than a high school diploma (Heflin & Iceland, 2009).
Not only do mentally disabled individuals face difficulty fitting into the workforce, they also are more likely to face sub-quality living conditions. In the United Kingdom, one in three households, housing a disabled person is considered to be substandard (Snell, Bevan & Thomson, 2015). These substandard conditions not only create a sense of dissatisfaction for those residing in such dwellings but also increase their susceptibility to chronic illness (Snell et al., 2015). These individuals’ increased susceptibility to illness is, in part, due to rising energy prices and the inability to afford heat and/or air conditioning (Snell et al., 2015). Because many of these individuals lack employment, it is assessed that more time is spent in the home, thus exacerbating the amount of time they are exposed to substandard conditions (Snell et al., 2015). Heflin & Iceland (2009) concluded that providing relief for energy costs and eviction prevention may have high social benefits, especially if provisions are extended to those within two hundred percent of the poverty line, as oppose to only those living in poverty.
The individual’s perception of their condition and the associated dissatisfaction both play a role in increasing the individual’s risk of experiencing depression (a degraded or impaired mental state) (Anakwenze & Zuberi, 2013). Depression can aggravate an existing mental health condition or in itself become a mental illness. The living conditions available to those with disabilities, including mental illness, is largely impacted by their ability to find and sustain employment providing the necessary income for suitable accommodations. The condition they find themselves in (i.e. facing mental illness, unemployment and poverty) is a cyclically diminishing one. It doesn’t take a John Maynard Keynes to understand that this cycle cannot recover itself efficiently.
Affording treatment
Well into the U.S.’s 2015 political debate season, a potential increase in minimum wage remains a pivotal topic. Many Americans are in favor of increasing the minimum wage standards, suggesting a societal need for increased income. To be clear, mentally healthy individuals making minimum wage claim to need more money. How can poor, mentally ill individuals, earning a subminimum wage afford treatment? The reality is that they likely cannot. But even if provided with income increases, mental health can only be improved by monetary gains if those gains are employed appropriately by the individual.
It has been suggested that an increase in minimum wage would improve mental health. This is largely based on research which has found positive correlations between income and mental health. Kronenberg et al. (2015) points out the expenses businesses can attribute to mental illness, such as absenteeism, and suggests that a minimum wage increase could improve mental health and productivity, thus becoming an affordable expense. While this logic may hold some merit, it is not determined if individuals would invest additional income towards improving their mental health and, moreover, there is a lack of empirical evidence to support such assumptions. It is determined, however, that disabled individuals, as compared to non-disabled individuals, face proportionally greater increasing living costs, are less likely to be employed, are less likely to be employed full-time (if employed), and receive lower wages (Snell et al., 2015).
In many instances, individual’s mental disorders go untreated. While this in itself is tragic and sometimes fatal, in impoverished communities it is more likely that a mentally ill parent’s interactions with their children be harmful. Not only do children in these situations grow up with the same economic insecurities, they are exposed to, and are affected by, the stress, anxiety, and depression present within the household. These situations have a biological effect on the brain and require treatment (Anakwenze & Zuberi, 2013). This needed treatment often doesn’t occur. In many cases, mental illness coupled with poverty leads to criminal activity and imprisonment. Harding suggests that a physiological mechanism exists by which the violence present within low income neighborhoods yields mental health concerns, such as chronic stress (as cited in Anakwenze & Zuberi, 2013, p. 150). These mental health problems undermine individual’s self-efficacy and perpetuate further negative consequences.
The socioeconomic issues covered herein do little to scratch the surface of what seems to be a nearly silent epidemic. Overshadowed by international threats, presidential debates and Hollywood shenanigans, the issue of mental illness has many socioeconomic implications. I suggest further research is needed in many areas related to mental health reform, to include: the role of mental illness concerning violent and juvenile offenders, neighborhood disorder (i.e. perceived levels of social support and integration), and the relationships between depression, aggression, addiction and trauma. The relationship between poverty, unemployment and mental health is complex, yet it can be reduced to a simple term, vicious circle. I conclude that mental health care in the U.S. is a substantial component to economic stability. Reformation of the economic strategy should include progressive government intervention in impoverished communities, to include crime prevention, education, job training and mental health rehabilitation and sustainment. Such programs create a demand for jobs and supply qualified job seekers. Long-term, such programs reduce crime rates and unemployment as well as have the potential to increase gross domestic product.
__________________________
References
Anakwenze, U., & Zuberi, D. d. (2013). Mental Health and Poverty in the Inner City. Health & Social Work, 38(3), 147-157.
Heflin, C. M., & Iceland, J. (2009). Poverty, Material Hardship, and Depression. Social Science Quarterly, 1051.
Kronenberg, C., Jacobs, R., & Zucchelli, E. (2015, Aug). The impact of a wage increase on mental health: Evidence from the UK minimum wage. Retrieved from http://www.york.ac.uk/media/economics/documents/hedg/workingpapers/1508.pdf
Mayo Clinic (2015, Oct 13). Mental Illness: Risk Factors. Retrieved from http://www.mayoclinic.org/diseases-conditions/mental-illness/basics/risk-factors/con-20033813
Snell, C., Bevan, M., & Thomson, H. (2015). Welfare reform, disabled people and fuel poverty. Journal Of Poverty & Social Justice, 23(3), 229-244. doi:10.1332/175982715X14349632097764
Ungar, M. (2014, Jan 12). Will a Higher Minimum Wage Make People Happier? [Web log comment]. Psychology Today. Retrieved from https://www.psychologytoday.com/blog/nurturing-resilience/201401/will-higher-minimum-wage-make-people-happier
U.S. Department of Labor (2008, Jul). Fact Sheet #39: The Employment of Workers with Disabilities at Subminimum Wages. Retrieved from http://www.dol.gov/whd/regs/compliance/whdfs39.pdf
 Jordache Williams is currently based in Rock Hill, SC and is a Licensed Professional Counselor with Atlas Concepts, LLC.
Jordache Williams is currently based in Rock Hill, SC and is a Licensed Professional Counselor with Atlas Concepts, LLC.